Is it possible to end mother-to-child HIV transmission in Nigeria’s oil-rich Rivers State? The inside story reveals explosive progress—yet, the full picture is more layered than you might imagine.
Imagine the hustle and bustle of a typical antenatal centre in Port Harcourt. Expectant mothers file in—some peeking nervously over colourful wrappers, others shielding their bumps from the midday sun. In a state where riverine communities stretch far and wide, reaching the next health facility can be as tricky as crossing Eko Bridge at rush hour. Still, an unprecedented 95% of these women have reportedly accepted HIV testing in Rivers State since 2020, according to the Institute of Human Virology Nigeria (IHVN).
The Inside Story: River State’s Fight Against Mother-to-Child HIV Transmission
Dr Stanley Idakwo, Project Director for the Rivers ASPIRE initiative at IHVN, didn’t mince words when briefing health stakeholders in Abuja. He described the achievement as the result of “years of strategic community engagement and persistent peer mentorship.” This isn’t just a big English, o! Data from the District Health Information System confirms it: HIV screening acceptance among pregnant women ranges from 95% to a whopping 100% over the last three years.
But what’s powering these results? Dr Idakwo attributes the change to a brilliant blend of effective counselling, robust peer support, and—perhaps most uniquely—mentor mothers. These are women living with HIV themselves, serving as beacons of hope and practical guidance. The strategy, he claims, “encourages adherence and emotional support.” No wonder over 98% of clients reportedly express satisfaction with the prevention of mother-to-child transmission (PMTCT) services provided.
What’s the Real Story Behind the Numbers?
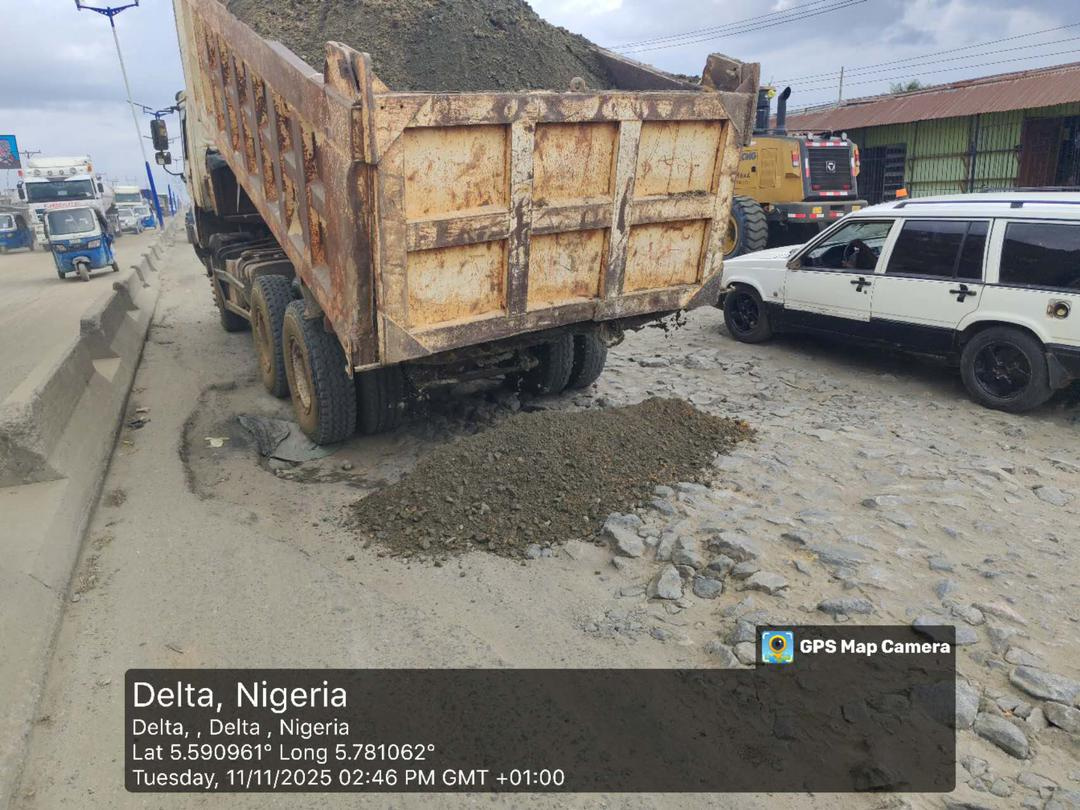
Of course, it wouldn’t be Naija if there weren’t some wahala along the way. Even with sky-high acceptance, challenges stubbornly remain. According to Dr Idakwo, “About 31.7% of women cited distance as a real obstacle. More than one in five mentioned transportation costs, while 16.5% pointed to long waiting times at clinics.” For many, travelling isn’t just about fuel scarcity—it’s about canoes, rough roads, and, sometimes, rain that won’t let up.
So how are health officials handling these issues? By sharing tasks among healthcare workers, managing cases more efficiently, and blending PMTCT into wider maternal and child health programmes, they’re making real progress. “Improved staff attitude and shorter queues mean more women now attend clinics,” Dr Idakwo remarked. Na so e suppose be!
Nigeria’s Mentor Mother Model: A Game Changer?
There’s something deeply powerful about seeing those who’ve walked your path guiding you, especially in a society where stigma can be more painful than any diagnosis. The mentor mother model reportedly does just that. Mentor mothers are said to encourage women to take medications and attend postnatal follow-up visits, reducing the risk of HIV transmission to their babies.
However, Dr Idakwo pointed out that while mother and infant antiretroviral (ARV) prophylaxis have slashed HIV transmission rates, not everyone sticks to the full regimen. There’s still room for improvement in follow-up services like hospital deliveries and ARV use during labour—vital steps in shattering the chain of transmission for good.
Pushing Boundaries: Health Access for Rivers’ Hard-to-Reach Areas
Reaching riverine and rural communities remains a stubborn bottleneck. But the ASPIRE Project is switching things up. By partnering with the Rivers State Ministry of Health, they’re expanding PMTCT access closer to remote communities. It’s not just talk: with support from the President’s Emergency Plan for AIDS Relief (PEPFAR-CDC) and the Global Fund, over 400 Traditional Birth Attendants (TBAs) have reportedly been trained. These TBAs now work hand-in-hand with 115 healthcare facilities, using a “hub-and-spoke” model to ensure women in 319 local wards don’t slip through the cracks.
This effort means women can now get quality, stigma-free care—from screening to delivery and even after childbirth. As one community leader in Tai LGA described it, “Back in the day, you go waka tire before you fit see doctor. Now, help dey near our backyard.”
How Are They Sustaining Progress?
- Continuous Training: Ongoing capacity building for community health workers and counsellors.
- Drug Supply Management: Improved logistics, so life-saving ARVs don’t finish at the crucial moment.
- Mentor Mothers and Midwives: Monitoring women through pregnancy, delivery, and the tricky postnatal period.
- Facility Upgrades: Extending PMTCT services beyond tertiary hospitals to primary healthcare centres.
- Safety Focus: Putting measures in place to protect health workers serving remote and, sometimes, volatile areas.
“Our ultimate goal is no child born with HIV in Rivers State. Every pregnant woman deserves excellent, stigma-free healthcare—whether she lives inside a city gate or across a river,” Dr Idakwo summed up in his Abuja address. For many families, these aren’t just statistics—they’re everyday realities and dreams for a healthier future.
Comparing Rivers State’s Progress: A Nigerian and African Perspective
You may wonder, is Rivers State alone in this battle? Not at all. According to World Health Organization data, several West African countries have ramped up mother-to-child transmission prevention. But Rivers’ 95%+ acceptance rate places it among the continent’s frontrunners.
Still, experts like Lagos-based public health analyst Mrs. Nkem Akintola caution that community buy-in, adequate transport infrastructure, and regular follow-up remain the foundation of sustainable success. “It’s not just about getting a woman tested once; it’s about walking the journey with her—every step of the way,” she explains.
What Lies Ahead for Mother-to-Child HIV Prevention in Rivers?
Looking ahead, it appears Rivers State is not slowing down. IHVN and the government are keeping their eyes on the ball—strengthening community partnerships, sustaining the mentor mother approach, and rolling out new strategies to connect even the most “faraway” families to care.
All these efforts point towards one fiery goal: a generation where HIV discharges no new chain through birth, and where every woman—no matter her address or wallet size—can step into motherhood with honour and hope.
Conclusion: Is Zero HIV Transmission from Mother to Child Now Within Reach?
With bold commitment and strong collaborations, Rivers State is telling a true Naija success story—one with its fair share of drama, determination, and hope. Still, the journey is not over. Will the rest of Nigeria follow Rivers’ lead to eliminate mother-to-child HIV transmission? Or, as we say, is this just the beginning of “better days ahead” for our mothers and children?
What’s your view on Rivers State’s PMTCT campaign? Which interventions do you think will most help mothers in your community? Drop your comments below and join the conversation.
Have insider news on healthcare, or want your voice heard in Nigeria’s HIV prevention journey? Share your story or sell your experience—email us at story@nowahalazone.com and shine a spotlight on real change. For support or tips, reach us at support@nowahalazone.com.
Follow us for the latest health updates and inspiring stories on Facebook, X (Twitter), and Instagram. Let’s make health news matter together!