Nigerians and their West African neighbours are facing renewed health challenges as the Africa Centre for Disease Control and Prevention (Africa CDC) has voiced growing concern about the return of cholera outbreaks and a rise in mpox (formerly known as monkeypox) cases across several African nations. The agency’s senior leadership, including Chief of Staff, Ngashi Ngongo, addressed these issues during a regional health briefing on Thursday, painting a complex picture of progress, setbacks, and urgent recommendations for the continent.
Cholera and Mpox Resurgence in West Africa: Latest Data
According to Africa CDC, while strides have been made in combating major outbreaks in some previously affected countries, fresh surges are now being observed, particularly in Liberia, Kenya, and Ghana. For Ghanaians, recent mpox statistics are cause for concern, with an average of 38 mpox cases recorded—most of which have been traced to the Western and Greater Accra regions.
Mr. Ngongo shared that these infections represent approximately 70% of all confirmed incidents linked to 3,449 identified contacts, 16 of whom have tested positive. To improve containment, Ghana is decentralising mpox testing across 15 regions, supported by the deployment of over 33,000 vaccine doses countrywide as of October 3rd. “Mpox testing in Ghana has now been decentralised across 15 regions, and the country began vaccination on 3 October with 33,000 doses deployed nationwide,” said Ngongo.
Rising Cholera Cases: Regional Trends and Contributing Factors
On the cholera front, the region has exceeded the total number of reported cases for 2023, reaching 272,324 by the 39th epidemiological week of 2024, according to Africa CDC data. This marks a pronounced increase compared to 254,075 cases the previous year. Disturbingly, the case fatality rate climbed from 1.9% to 2.3% within the same period—meaning nearly 3 out of every 100 infected individuals did not survive the infection.
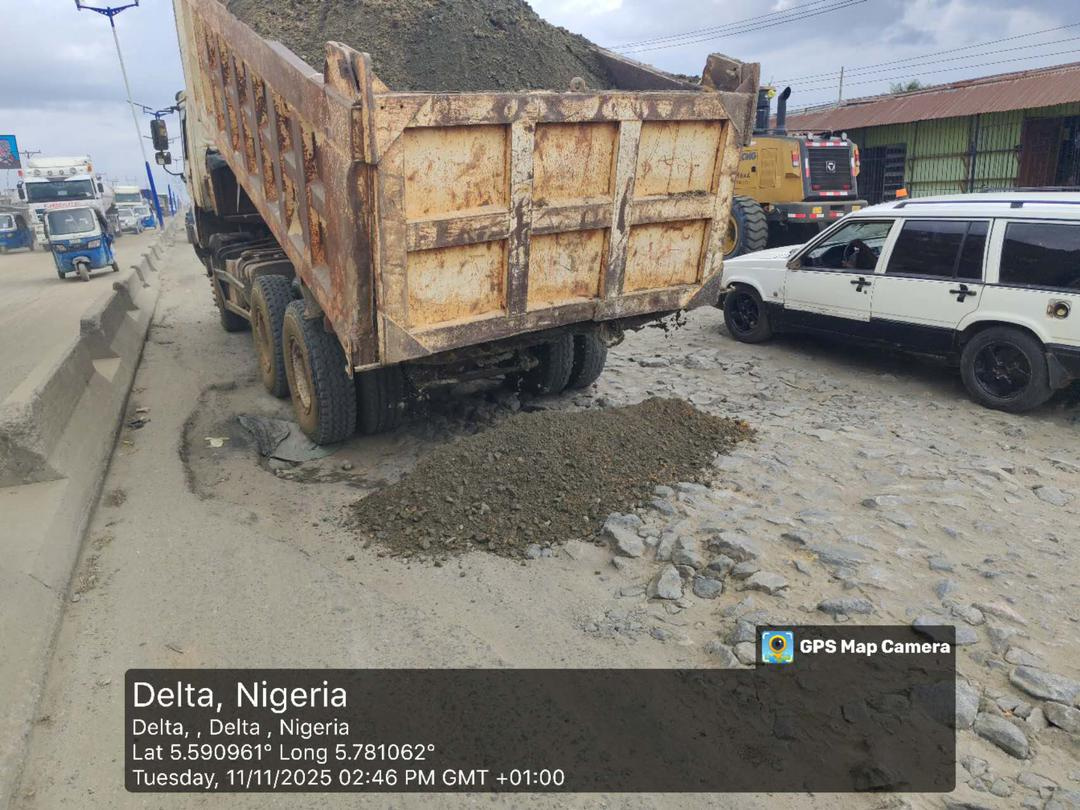
Currently, 23 African Union member states are affected by cholera, with 17 actively battling outbreaks. As the rainy season arrives in many countries, Africa CDC warns that the trajectory may grow even steeper, as heavy rains tend to accelerate cholera’s spread by contaminating local water supplies.
Chad, Angola, and Burundi are among the nations experiencing the sharpest uptick in cholera transmission, each reporting surges exceeding 160% between epidemiological weeks 34 and 39 (compared with the preceding six weeks). Angola’s situation has drawn particular attention, as several new hotspots have emerged in its northern and eastern provinces, including Lunda Norte, Nuich, and Willa. This comeback happens despite over two million oral cholera vaccine doses being distributed during earlier campaigns in July 2024.
According to Ngongo, “Unsafe water, poor sanitation, and outbreaks in mining and river-dependent communities remain key drivers of the epidemic in Angola.” For Burundi, cases rose by 26% since week 29, although, as at the time of reporting, no fatalities were recorded. Local health officers cite water scarcity, poor hygiene infrastructure, and significant cross-border movement—particularly from the Democratic Republic of Congo—as leading causes behind the continued spread.
Broader Health Implications and Emerging Threats
The resurgence of these infectious diseases underscores Africa’s ongoing struggle with public health emergencies that can escalate quickly, threaten lives, and overburden already stretched health systems. According to Abuja-based epidemiologist Dr. Ifeoma Okeke, “When routine sanitation collapses due to flooding, rapid urbanisation, or displacement, outbreaks flourish—and no region, from the coast of Lagos to Accra’s city slums, is immune.”
Ngongo and other officials also highlighted emerging threats such as Rift Valley fever in Senegal and Mauritania, showing the interconnectedness and mobility of tropical infections. Encouragingly, the Democratic Republic of Congo has reported no new mpox cases for ten consecutive days, serving as a positive sign for the region. Most recent outbreaks have been linked to animal-to-human transmission, spotlighting the urgent need for holistic strategies like the “One Health” approach, which integrates the wellbeing of people, animals, and their shared environment.
African Solutions for African Challenges: Calls for Vaccine Sovereignty
One persistent challenge is access to medical countermeasures—including vaccines, therapeutics, and diagnostics. “This is why we need to step up research, development, and local manufacturing to ensure Africa produces its own vaccines, therapeutics, and diagnostics,” Ngongo stressed. The COVID-19 pandemic starkly revealed the risks of relying on external sources for critical health supplies, motivating several African countries—including Nigeria, Ghana, and South Africa—to invest in local pharmaceutical production. Africa CDC’s newly signed partnership framework with the World Health Organization (WHO) is expected to enhance regional response coordination and resource-sharing.
Understanding Mpox and Cholera: Symptoms, Spread, and Prevention
Mpox, which the World Health Organization renamed from monkeypox to curb stigma, is caused by the mpox virus. The illness often begins with fever, headaches, muscle pains, and swollen lymph nodes before progressing to a distinctive rash resembling—though milder than—smallpox. Transmission is primarily through close contact with an infected person or animal, or contaminated items. Recently, mpox outbreaks have increased globally. Experts attribute this to waning immunity since the eradication of smallpox decades ago and the discontinuation of mass smallpox vaccinations that previously provided cross-protection.
Cholera, on the other hand, is an acute diarrhoeal disease caused by the bacterium Vibrio cholerae. People typically become infected through contaminated food or water, making vulnerable populations—such as those without safe drinking water or adequate sanitation—especially at risk. If not quickly treated, severe cases can lead to dehydration, shock, and even death. However, rapid detection, access to safe water, improved sanitation, and timely medical treatment dramatically boost survival rates, according to the Nigeria Centre for Disease Control (NCDC).
Impact on Nigerians and West Africans: Local Voices & Realities
In communities like Lagos’ Makoko, where riverside shanties meet crowded walkways, the risk is palpable. “Whenever the rains start, we’re scared of cholera,” says Mrs. Oluchi Chukwu, a local youth leader. “Children fall sick easily, and sometimes, clinics can’t handle all the patients.” In northern Nigeria, communities near major rivers face similar challenges, as noted by public health nurse Aisha Shehu from Zamfara: “Every year, we ask for more clean boreholes, but some villages still rely on streams, which puts everyone at risk.”
Many urban West Africans, especially in big cities like Accra, Lagos, and Abidjan, now follow health updates on social media platforms and via government alerts. Regional responses—such as Ghana’s rollout of decentralized mpox testing and Nigeria’s improved deployment of oral cholera vaccines—show encouraging signs. However, health experts urge that these efforts must be sustained and inclusive, reaching both rural and hard-to-access populations.
State of Preparedness and the Next Steps
Success in containing infectious disease outbreaks hinges not just on providing emergency vaccines but on strengthening the entire health system. Dr. Daniel Mensah, a Ghanaian public health consultant, notes, “Without reinforcing our clinics, training more disease detectives, and investing consistently in clean water infrastructure, these cycles of outbreak will keep repeating themselves.” Continued investment in health education—empowering people with knowledge on sanitation, vaccination, and early symptom recognition—is crucial.
Africa CDC’s leadership has welcomed deeper collaboration with global partners, especially the World Health Organization. “Partnerships will help advance stronger, more integrated, and better coordinated responses to multiple health events,” said Ngongo. But independent, locally tailored solutions—championed by local health agencies and community leaders—remain just as essential on the ground.
How Can Communities Protect Themselves?
- Prioritise drinking treated or boiled water, especially during the rainy season
- Wash hands frequently with soap and safe water
- Report cases of sudden diarrhoea or unusual rashes promptly to health authorities
- Participate in vaccination campaigns when available
- Encourage local governments to invest in safe water and improved sanitation facilities
While Africa grapples with old and new disease outbreaks, the resilience, vigilance, and cooperation of local communities remain a key defence. As government agencies and health experts increase efforts, everyday Nigerians and West Africans can help by staying informed and adopting preventive practices in their neighbourhoods and workplaces.
What has your community done to address health risks like cholera and mpox? Do you think more can be done at the local or regional level? Share your thoughts below and follow us for reliable updates and powerful African stories!
For general support, questions, or feedback, reach us directly at support@nowahalazone.com.
Stay connected with us on social media for the latest Nigerian and West African health news—follow us on Facebook, X (Twitter), and Instagram.
Your perspective matters—join the conversation, share your story, and help build a healthier Africa!